We chatted to Senior House Officer aka Doctor, Stephanie about what it’s like to hit the ward on the daily and how she knew being a doctor was the way to go.
Here it is:
FN: What’s the grossest thing you’ve seen?
S: I’ve seen limbs sticking out at completely wrong angles and been sprayed in the face with blood but honestly, pus, vomit and diarrhoea are the worst. No matter what, they never stop being gross.
FN: What is your official title and what does a typical day look like for you?
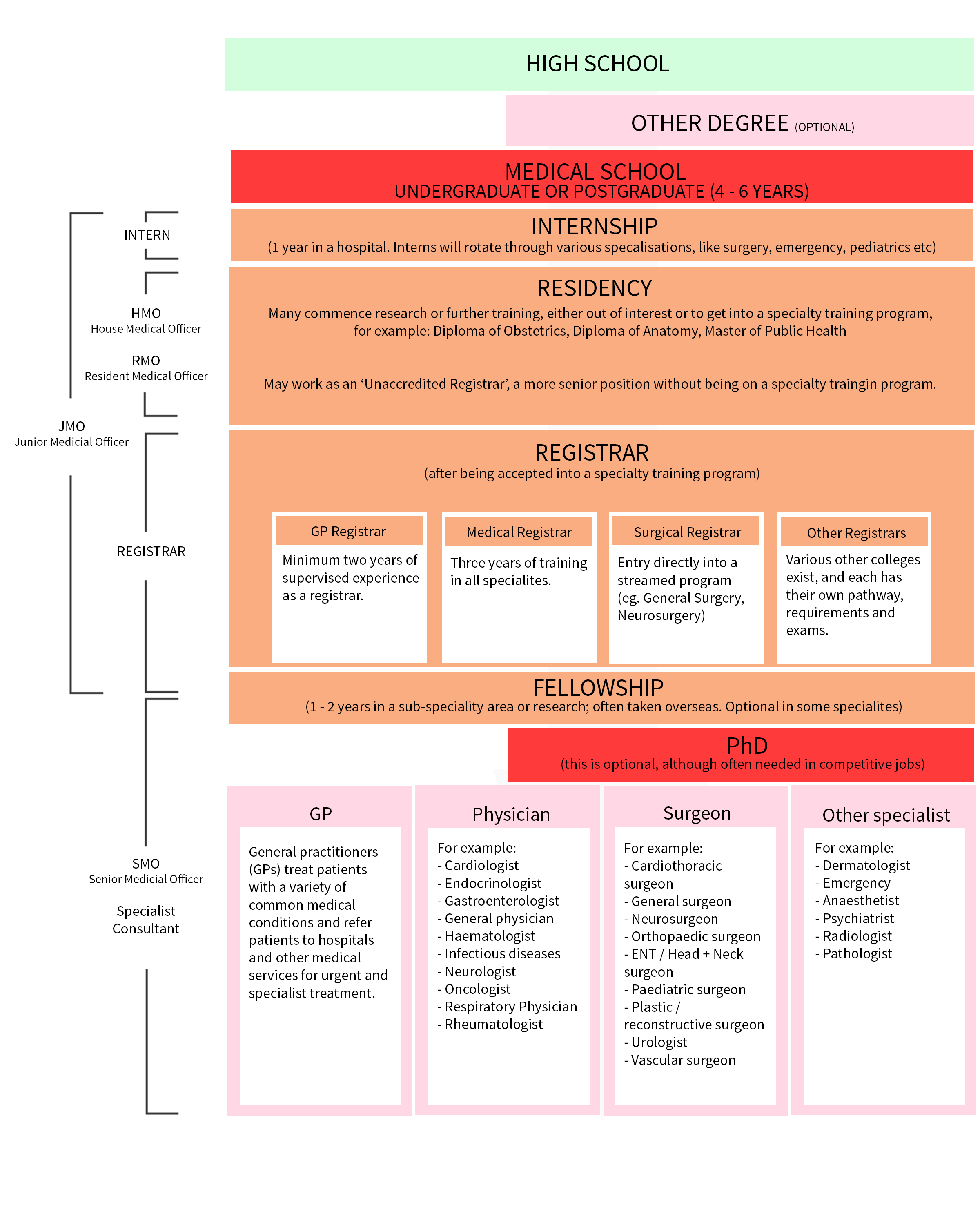
S: My official title is ‘Senior House Officer’ (usually abbreviated to SHO) which is a type of Resident a.k.a hospital doctor in training who hasn’t necessarily decided what they’d like to specialise in just yet.
This means I’ve finished my intern year (yay!) and worked for at least one year (as a Junior House Officer, also a type of Resident). The terminology is a bit clumsy thanks to the British hospital system.
Throughout training we’re rotated through various parts of the hospital so we can be exposed to different areas before choosing a specialty. We usually spend two to three months in each area before moving on.
I want to be a Physician (as opposed to a Surgeon) – think a House-type doctor rather than a Grey’s Anatomy doctor.
This means that through the years I’ve chosen to work in more medical rather than surgical areas. This suits me because I’m not a fan of the early starts and long days in surgery.
FN: What would you describe as your ‘office desk’?
S: Regardless of whether you’re doing Medicine or Surgery, the day will start with a ward round. This is where the team of doctors walks around the hospital and visits their patients to see how they’re going as well as discuss results and plan ongoing treatment and investigations.
Before the ward round it’s the responsibility of the Resident to update the patient list. They’ll be taking notes, checking observations, overnight events, reviewing medications and arranging tests. For urgent matters this can mean ducking out to make phone calls or running halfway across the hospital to organise things in person. Anything not done during the round goes on a jobs list for later on.
FN: What’s the biggest misconception about your career?
S: The rumours are mostly true. Doctors work hard but because we work in teams, it’s actually a lot of fun and very social. Colleagues often go out of the way to support you; there’s a lot of good karma going on!
I also find that just because I’m young and a woman does not mean that I’m a) too young to know what I am doing, or b) a nurse. Newsflash – not all women are nurses and not all men are doctors (and we all carry stethoscopes).
This is an almost universal experience for female doctors and I‘ve seen people refuse to be treated by even very experienced female clinicians. I’m almost excited for my first grey hair and wrinkle to appear to avoid this! Just kidding…sort of.
FN: What career hurdles have you had to jump?
S: Getting into med school. For me, this meant applying to universities around the country and moving interstate to study. Doing this straight after finishing school was a bit daunting at first but one of the best things I’ve ever done.
After this came my internship year which involved regular assessment and reflection on my clinical work with supervisors.
The next big thing on my horizon is preparing for the Divisional Written and Clinical Examinations a.k.a the hardest exam you will ever sit. EVER. Thankfully, they should hopefully also be my last!
FN: How/Why did you decide to become a doctor?
S: It’s hard to know exactly. [I think] a small amount of kindness can make even unbearable circumstances just a tiny bit less awful!
FN: What do you love about your job/career?
S: The people! Medicine is a career where you’re privileged with sharing major life events with your patients. You see babies born and sit with families while their loved one dies.
You see the best of people but also the worst. People’s resilience and wisdom will never cease to amaze me.
The other really attractive thing about medicine is that it’s challenging. It’s about thinking and problem solving and really is a career of lifelong learning. This might not suit everyone but I find this really rewarding and invigorating.
FN: How do you separate work and home in what can be a highly emotional workplace?
S: Sometimes it’s really hard. Reflecting on the day and the decisions you have made is not necessarily a bad thing (in fact, it’s super important) but if something is plaguing you or causing you to lose sleep, that’s obviously not healthy.
In my experience, when big things happen at work it’s often emotional for everyone, and the concept of debriefing (both formally and informally) is fairly well established within the profession. It definitely helps. I think balancing work with a few activities helps as well. I play in a social touch football competition and play guitar in my church’s music team. I also enjoy running and have recently started working mindfulness meditation into my day.
FN: At what point are you considered a stand-alone, ‘proper doctor’; no supervision required?
S: Theoretically after you pass your intern year and receive your general registration you don’t require supervision to practice. In reality if you wish to specialise (including becoming a GP, surgeon or physician) you need a minimum of 4 to 10 years (sometimes more) of supervision and have to pass a few exams before you’re a consultant/specialist/‘proper doctor’.
TF: What qualifications and education do you have?
S: I finished my Higher School Certificate in New South Wales before studying a combined Science and Medicine Bachelor’s degree (BSc/MBBS) at the University of Queensland.
FN: How long did university take? Did you see this length as a deterrent when deciding on your career?
S: I completed six years of study at University for a dual degree in Science and Medicine (BSc/MBBS). Although the medical program at the University of Queensland is technically classified as post graduate, the University offered a certain number of places with guaranteed direct entry from high school after the completion of an accelerated two years of an undergraduate degree. This has recently changed and you have to do all three years of an undergraduate degree.
Although there are a few different types of Medical Degrees in Australia (if you ignore the name of the qualification, the biggest difference is undergraduate versus post graduate entry), graduates from all programs come out with a couple of years of predominantly theoretical study and a couple years of clinical placement.
It seems like a lot of time to spend at Uni but I was certain I wanted to be a doctor when I left school and I really enjoyed my time so it didn’t bother me too much (although I was grateful to kiss exams and assignments goodbye when I did).
Keen to become a doc? Head to our course finder to get started.